At SpecialEyes, our highest priority is helping you obtain successful patient outcomes. As you probably know, the leading cause of contact lens dropout is discomfort. (1) While our material is known for its biocompatibility and excellent water retention, comfort issues may still occur. Let’s take a look at some of the underlying causes of discomfort and best practices for troubleshooting these issues.
Causes of Contact Lens Discomfort
Due to the variety of potential causes, comfort issues can be difficult to troubleshoot. As you fit the lens on your patient’s eye, it’s important to think about the variables that could cause discomfort for your patient. Common reasons for discomfort are:
- Lens fit (too tight or loose)
- Everted lens
- Lens size
- Solution sensitivities
- Lens care and compliance
- External environment
- Defective/torn lens
- Lens material
- Ocular conditions
- Systemic conditions
- Certain medications
Lens Awareness
Contact lenses interact with some of the most sensitive areas of the body, such as the cornea, lid margin, and conjunctiva. Because of this, the eye can detect the presence of the contact lens. If your patient is new to wearing lenses or hasn’t worn contacts in a long time, it is possible they will mistake lens awareness for discomfort. Upon initial insertion, it is not uncommon for some patients to report a minimal amount of lens discomfort. However, this feeling should subside within the first few minutes of wear time as the eye becomes accustomed to the lens. One way to help minimize or eliminate this initial lens awareness is to rinse the lenses with a multipurpose solution prior to insertion and make sure the patient does not have the lens everted. SpecialEyes contact lenses are shipped in vials filled with a sterile, buffered saline solution. Although this solution is safe for an ocular environment, it can sometimes cause initial irritation, foreign-body sensations, or burning. If the patient still reports discomfort after taking this precaution, you should suspect that the lens is too flat, too thick, or has a torn edge.
Tight Lens Discomfort
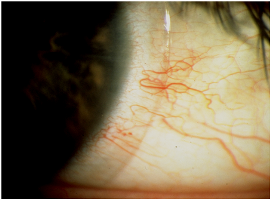
Tight lenses tend to feel comfortable upon initial insertion; however, they can lead to discomfort after multiple hours of wear time. Since tight lenses do not move much on the eye, tear exchange is often poor, which can result in lens dehydration. When this happens, patients may report that their eyes feel itchy or dry; and in most cases, they will experience reduced visual acuity as the day goes on. Upon follow-up, you may even observe scleral indentation or conjunctival drag. (2) Conjunctival drag means that the lens is so tight that it pulls the conjunctival membrane during the blink or push-up test, causing irritation and redness. When this occurs, you can correct the problem by changing the base curve and/or diameter to improve the fit.
Chronic Dry Eyes
Patients with chronic dry eyes are unable to produce enough tears to keep their eyes moist. This dryness can be caused by a medical condition, certain medications, or acquired through risk factors like smoking, computer use, caffeine, etc. With over 4.88 million people in the U.S. suffering from chronic dry eyes (3) and nearly 45 million contact lens wearers nationwide (4), you’re likely to run into a patient with this problem. If your patient experiences discomfort from chronic dryness in a lens with low wettability, you may want to consider a lens with a higher permeability (Dk). For example, SpecialEyes 59% material has a Dk of 24, which helps keep our patients with chronic dry eyes happy and comfortable.
Lens Care and Compliance
According to the Centers for Disease Control and Prevention (CDC), 40% to 90% of contact-lens wearers do not follow proper lens-care instructions given by their practitioner. (5) Non-compliance goes beyond not cleaning and disinfecting the lenses; other examples include wearing lenses beyond their replacement schedule, sleeping in daily-wear lenses, improper use of solutions and care products, and switching care regimens without speaking to an eye-care provider. When contact lenses are not properly cared for, patients can experience discomfort and reduced vision, and may face potentially damaging adverse reactions.
Here are some tips you can share with patients to promote healthy lens-care habits; you may want to provide them with a printed copy as a take-home checklist:
- Handling contact lenses with clean hands is the first step in healthy lens wear. Always wash hands thoroughly with a mild, non-oily soap, rinse well, and dry using a lint-free towel.
- When preparing to insert a lens, tip the lens into a palm and then gently place it on the eye with the pad of a finger. Never use fingernails or tweezers to remove a lens from the vial or contact lens case.
- When removing a lens from the eye, first apply a rewetting drop and then gently slide the lens out using the pad of a finger.
- Immediately after removing a lens, be sure to always clean, rinse, and disinfect it, and neutralize if using a hydrogen peroxide system. SpecialEyes also recommends lightly rubbing (not scrubbing!) the lenses during cleaning, even if the solution is advertised as a “no-rub” formula. Proper cleaning and disinfection are important, since mucus, bacteria, secretions, films, and deposits that develop during wear can lead to discomfort, reduced vision, and infection.
- Never sleep in SpecialEyes contact lenses. SpecialEyes lenses are not approved for overnight wear and should be removed before sleeping. Leaving non-approved lenses on the eye overnight significantly increases the risk of conditions such as hypoxia (oxygen deprivation in cells), corneal ulcers, and infection. In fact, according to the CDC, patients who sleep in contact lenses are at 8 times greater risk for an eye infection. (6)
- Use the solutions and lens-care products recommended by your eye-care professional. Carefully read and follow the products’ instructions. Generic solutions may contain different ingredients and preservatives that deviate from the name brand’s current formula. To avoid an adverse reaction linked to solution sensitivity or incompatibility, always consult your eye-care professional before switching to a different solution or lens-care product.
- Always use fresh, unexpired solution. If old solution is reused or topped off, contact lenses may become contaminated with debris or bacteria that can cause serious eye infections.
- Replace contact lens cases regularly. To avoid contamination and infection, contact lens cases should be cleaned using fresh lens solution and replaced at least every three months.
- Never clean, rinse, or store contact lenses in water. Even purified water is full of microorganisms that can contaminate and damage lenses, leading to infection or injury.
- Follow the prescribed lens replacement schedule. Though it may be tempting to try to prolong the life of your lenses, don’t do it! Extending the replacement period can cause reduced comfort and visual acuity, and may lead to an infection.
Questions to Ask the Patient
The following questions can help you pinpoint what may be causing your patient’s contact lens discomfort:
- Does the discomfort occur immediately upon insertion or later in the day?
- Does comfort improve or get worse with wear time?
- How would you describe the discomfort? For example, is it an awareness of the feeling of the lens on your eye? Or is it more of a scratchy, burning, or dry sensation?
- What lens-care products are you using?
- Describe your daily lens-care routine.
- What kind of environment(s) are you usually in at home, work, and in your free-time activities? Do you encounter dry, dusty, cold, or windy conditions on a regular basis?
- Do you have any systemic conditions or take any medications?
Once you have answers to the above questions, be sure to evaluate the lens fit for good centration, movement, and limbal coverage. Note any issues with corneal health or ocular pathology. Then, contact the SpecialEyes consultation department. Our consultants are experts in making lens adjustments to ensure your patient has crisp vision and a comfortable lens wear experience.
Resources
(1) “Discomfort: Leading Cause of Contact Lens Dropouts”; Review of Optometric Business; December 10, 2012. https://www.reviewob.com/discomfort-leading-cause-of-contact-lens-dropouts/
(2) Yanoff, Myron, Jay S. Duker, and James J. Augsburger. Ophthalmology; Edinburgh: Mosby Elsevier; 2009. http://www.clinicalkey.com/dura/browse/bookChapter/3-s2.0-B9780323043328X00017
(3) American Academy of Ophthalmology. “Eye Health Statistics: Eye Diseases”; accessed August 7, 2020. https://www.aao.org/newsroom/eye-health-statistics#eyediseases
(4) Cope, Jennifer R., Sarah A. Collier, et al. “Risk Behaviors for Contact Lens–Related Eye Infections Among Adults and Adolescents — United States, 2016”; Morbidity and Mortality Weekly Report (MMWR); August 18, 2017. https://www.cdc.gov/mmwr/volumes/66/wr/mm6632a2.htm
(5) Bui, Thai H., H. Dwight Cavanagh, and Danielle M. Robertson. “Patient Compliance During Contact Lens Wear: Perceptions, Awareness, and Behavior”; Eye Contact Lens; vol. 36, 6; 2010; pgs. 334–339. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3148150/
(6) Cope, Jennifer R., Nuadum Muriel Konne, et al. “Corneal Infections Associated with Sleeping in Contact Lenses — Six Cases”; Morbidity and Mortality Weekly Report (MMWR); August 17, 2018. https://www.cdc.gov/mmwr/volumes/67/wr/mm6732a2.htm